In many ways, 2022 may be looked back upon as a pivotal year. Following the initial surge of COVID-19 in 2020, the height of the pandemic and dramatic shifts in health care utilization in 2021, 2022 brought a renewed focus on issues such as disease prevention, health equity, mental health and virtual care.
And while COVID-19 remains a pressing global health issue, as the nation (and world) adapted to the “new normal” there were several encouraging developments in the areas of wellness, health equity and addressing social factors that hinder access to care.
Here are a few of 2022’s developments that will have an effect in the year ahead.
Washington puts a spotlight on hunger, nutrition and health
Perhaps the biggest story related to nutrition was the September 28 White House Conference on Hunger, Nutrition, and Health, the first such gathering in over 50 years. Catherine Macpherson, senior vice president of healthcare strategy and chief nutrition officer at Mom’s Meals®, was among those invited to the conference and participated in working group sessions where experts discussed questions posed by a moderator from the Department of Health and Human Services (DHHS).
The Biden administration said it will work with Congress to test medically tailored meals for the Medicare population, and test Section 1115 Demonstration waivers for medically tailored meals in the Medicaid population. If adopted as policy, both options would expand medically tailored meals to most people covered by a government payer.
Going forward, Macpherson believes there will be changes to food labels and the Dietary Guidelines for Americans, and we may see a new single institute governing nutrition policy and programs — spanning several agencies including the U.S. Department of Agriculture (USDA), DHHS and U.S. Food and Drug Administration (FDA).
Building on the momentum of the White House event, a few weeks later the USDA hosted Come to the Table: USDA’s National Nutrition Security and Healthcare Summit. More than 200 health care, federal and community leaders came together to advance the conference goals of ensuring all Americans have the resources necessary to eat nutritious foods that support good health.
There will be regional follow-up summits across the U.S. in 2023, with the aim to alleviate hunger and reduce burden of diet-related diseases.
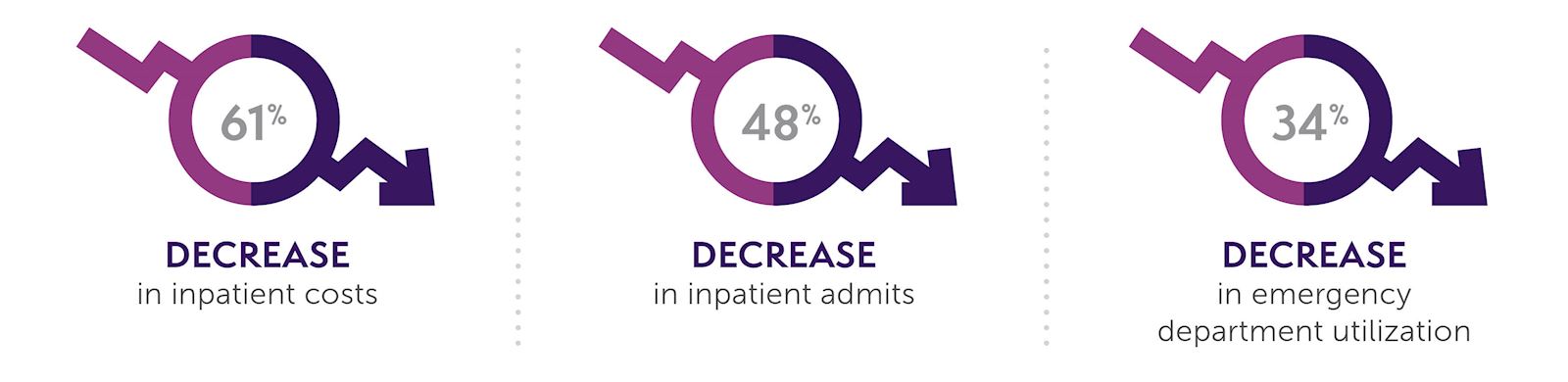
And just how costly is diet-related illness? The issue was put into perspective by a Tufts University study that estimated in addition to net cost savings of $13.6 billion for payers, national expansion of medically tailored meals for patients with diet-sensitive conditions and activity limitations could help avert 1.6 million hospitalizations annually.
Centers for Medicare & Medicaid Services (CMS) emphasizes patient experience in star ratings

According to its Contract Year 2022 Medicare Advantage and Part D Final Rule, CMS doubled the weight of patient experience measures used to calculate star ratings. This means patient access to care and experience will carry even more weight than outcome measures when calculating star ratings. Although this change will impact star ratings for plans in 2024, those ratings will be based on care delivered in 2022.
Other star ratings changes announced in 2022 that will impact 2023 ratings include the Controlling Blood Pressure measure, which moved into the 2023 star ratings as a new outcomes measure.
As part of its health equity framework, CMS now requires the collection and reporting of standardized fields for race, ethnicity, language, gender identity, sex, sexual orientation, disability status and Social Determinants of Health (SDOH). In September, the agency released a Request For Information (RFI) seeking public input on accessing health care and related challenges, understanding provider experiences, advancing health equity, and assessing the impact of waivers and flexibilities provided in response to the COVID-19 Public Health Emergency. Data gathered will help determine how programs and policies affect health inequities and health disparities.
In addition to the star rating changes, CMS made several changes to MA policy, including:
- Value-Added Items and Services can now be mentioned in the Medicare Summary of Benefits, so health plans can communicate about health-related products or services to enrollees that add value to, but are not part of, a plan of benefits.
- All Medicare Advantage Special Needs Plans (C-SNP, I-SNP, D-SNP) are now required to screen for SDOH needs, including food insecurity.
Updated NCQA HEDIS Measures
Each year, the National Committee for Quality Assurance (NCQA) updates measures in the Healthcare Effectiveness Data and Information Set (HEDIS) to ensure that they remain relevant and feasible for implementation. Updates in 2022 for 2023 include:
- ED Visits for Hypoglycemia in Older Adults with Diabetes (EDH) — Older adults are more likely to experience severe hypoglycemia, which can lead fall-related events, fractures, increased risk of cardiovascular events, and cognitive decline. Health plans have an opportunity to identify their older patients with diabetes who are at highest risk of hypoglycemia and implement preventive interventions.
- Social Need Screening and Intervention (SNS-E) — NCQA developed this measure as part of an organization-wide effort to advance health equity and encourage health plans to assess and address the food, housing and transportation needs of their patient populations. Health plans can identify specific needs and connect members with the resources necessary to address unmet social needs.
Home-delivered meals can positively impact star ratings
A home-delivered meals program can give your health plan a quality boost and contribute to star ratings improvement. For example, condition-appropriate, home-delivered meals can help people with diabetes keep their blood sugar controlled — an important quality metric in star ratings as a triple-weighted measure. When someone is well-nourished, their risk of falling decreases, and their physical health improves — other important quality measures.
 Source: https://www.ajmc.com/view/simply-delivered-meals-a-tale-of-collaboration
Source: https://www.ajmc.com/view/simply-delivered-meals-a-tale-of-collaboration
Mom’s Meals — Continued focus on quality nutrition for better health
Throughout 2022, Mom’s Meals continued its work to demonstrate the power of nutrition to help improve health and cost outcomes. In addition to its ongoing community-level work through initiatives including Iowa Stops Hunger, Hunger Challenge and the Community Champion Award program, the company embarked on a number of pilot programs to improve members’ health with diet. Programs included:
- Behavioral Health Pilot with UHC WI — UnitedHealthcare Wisconsin (UHC WI) and Mom’s Meals collaborated on a pilot program to support high-risk members with a behavioral health diagnosis by meeting their basic need for nutrition. In the pilot, 96 UHC WI members received three condition-appropriate, home-delivered meals for 90 days.
- Congestive Heart Failure pilot with IEHP — Inland Empire Health Plan (IEHP) and Mom’s Meals partnered in a pilot program to improve the health of IEHP members through better access to nutritious food, nutritional education and improved monitoring.

- Diabetes pilot with UHC HPN — Health Plan of Nevada, a UnitedHealthcare Company, partnered with Mom’s Meals on a pilot program to support diabetes management by better engaging its members and addressing food insecurity and social determinants of health.

Resources to help make a difference
As we move into 2023, we’ll begin to see the influence of all these regulatory developments, government engagement and pilot programs.
- For more detailed information and resources to help improve health and cost outcomes use our Guide for Medicare Advantage Plan Product Teams
- Discover how a home-delivered meals program can help enhance your plan’s star ratings
If you need more guidance on adding home-delivered meals to your MA plan and want to help boost your star ratings, Mom’s Meals is here to help. Our experts can work with you to design a food and nutrition benefit for your members. Contact us.

.jpg)