Managed care organizations (MCOs) have traditionally focused on providing medical benefits such as doctor’s visits, hospitalizations, and prescription medications to care for members facing illness or injury. But as research grows on how social determinants of health (SDOH) impact health and well-being, managed Medicaid plans, as well as states administering Medicaid programs, are looking for ways to implement innovative, new benefits to help their members proactively address members’ unmet health-related social needs (HRSN).
Now the Centers for Medicare & Medicaid Services (CMS) is supporting some of those efforts by state Medicaid programs. With CMS approval, ILOS allow plans to substitute services or settings covered in a state Medicaid plan because they are medically appropriate and cost-effective alternatives to traditional benefits.
State ILOS examples
New York now has a state-wide medically tailored meal (MTM) ILOS program for high-need individuals and is launching a recently approved 1115 demonstration that will address SDOH and advance health equity. Included in the program are a number of services to address HRSN, including MTM, as well as support for greater integration between primary care providers, community-based organizations and behavioral health specialists. HRSN will go live in late 2024.
Iowa is expanding its HRSN footprint in a groundbreaking ILOS approval for MCO members who are on a 1915(c) home and community-based services (HCBS) waiver waiting list and not currently receiving these services. The MCOs now have authority to provide many long-term services and supports waiver services including MTMs.
CMS approved a proposal by California’s Medicaid plan, called Medi-Cal, to use Community Supports (California’s nomenclature for the proposed list of state-approved ILOS) to offer a set of 14 health-related, non-medical services to members. California is a vanguard when it comes to ILOS, but awareness and interest in the option is growing.
14 approved Community Supports in California
- Housing Transition Navigation Services
- Housing Deposits
- Housing Tenancy and Sustaining Services
- Short-Term Post-Hospitalization Housing
- Recuperative Care (Medical Respite)
- Day Habilitation Programs
- Caregiver Respite Services
- Nursing Facility Transition/Diversion to Assisted Living Facility
- Community Transition Services/Nursing Facility Transition to a Home
- Personal Care and Homemaker Services
- Environmental Accessibility Adaptations (Home Modifications)
- Asthma Remediation
- Medically Tailored Meals
- Sobering Centers
ILOS benefit to members
Members benefit from ILOS because they can have access to helpful services that address needs and improve health, such as condition-specific nutritious home-delivered meals, asthma remediation and home modifications. Under CMS rules, health plans can offer innovative services that help meet a person’s unique needs, particularly related to SDOH and health equity concerns.
ILOS benefit to health plans
CMS’ support of approved ILOS benefits is good news for managed care plans too. This benefit flexibility allows plans to focus on preventative solutions to keep members healthy and out of the hospital, which could improve outcomes and reduce costs. ILOS expenditures qualify as covered services for rate-setting, meaning their claims count toward the capitation rate. In addition, when ILOS are used to reduce waiting lists for other waivers, such as HCBS waivers, health plans not only can address the needs of members in a timelier manner, but they can also improve health outcomes and quality of life for members while reducing Medicaid spend.
How do it work?
There is no set list of ILOS benefits states can offer. Rather, it’s up to a state to seek CMS approval for services it proposes that are medically appropriate and cost-effective substitutes for Medicaid services. CMS approved a range of ILOS in California including nutritious meals, caregiver respite, home modifications, sobering centers, and more.
IEHP Pilot
A pilot program launched in 2021 between Inland Empire Health Plan (IEHP) in California and Mom’s Meals® demonstrates how a preventative program leveraging a service that addresses both a clinical need and a social need can work effectively to improve the health and lives of members.
The pilot's goal was to improve IEHP members' health through better access to nutritious food, nutritional education, and improved monitoring. Dually eligible members in certain counties with congestive heart failure (CHF) and a minimum of two previous hospital stays within the prior 12 months received home delivered meals from Mom’s Meals for 24 weeks. They also received nutrition counseling, support from community health workers and nurse case managers, exterior safety checks of their homes, and in-person wellness surveys, as well as produce and pantry boxes from Mom’s Meals for 12 weeks. The pilot was a success and achieved:
- 50% reduction in hospitalizations
- $1,613 per member per month savings on health care costs
- 5.8-pound average weight loss per participant
- 95% overall program satisfaction from participants
Reanalysis shows lasting impact
Data for 93 enrolled members was reanalyzed 6 months after first analysis; 12 months after program end date and found the program had a lasting impact:
- 42% reduction in hospitalizations
- 39% reduction in length of stay
- 21% reduction in total cost of care
Members also self reported:
- Improved access to healthy foods and lower salt consumption
- Reduced HF symptoms such as shortness of breath and swelling
Mom’s Meals – your ILOS partner
As the leading national provider of home-delivered, medically tailored meals, Mom’s Meals is a valuable resource when it comes to developing strategies to promote ILOS. Rely on our expertise in partnering with managed care organizations and State Departments of Health in California, New York and other states to help inform your program.
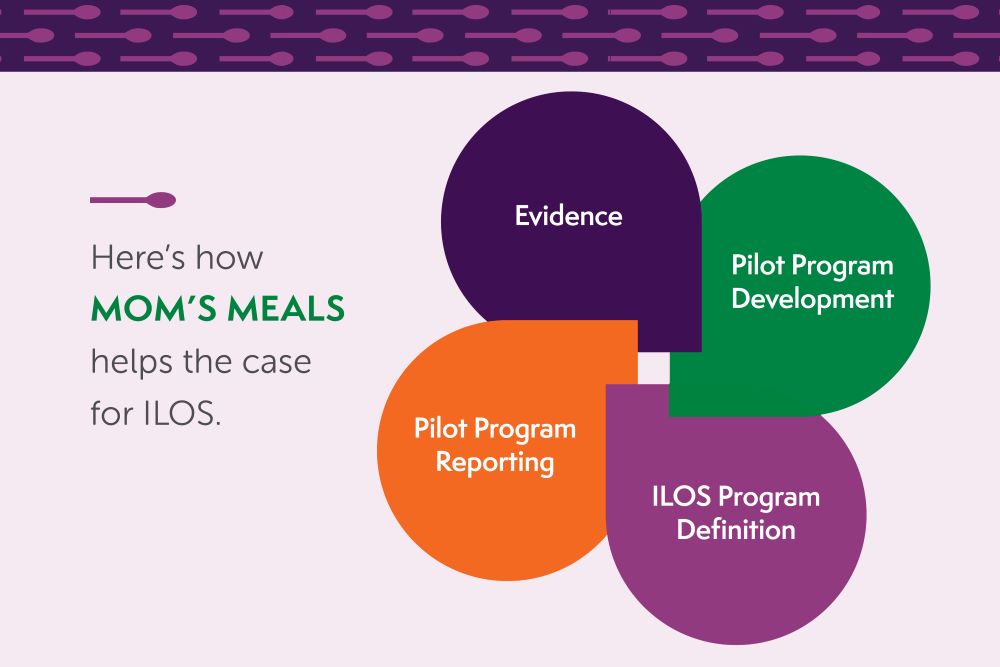
How Mom’s Meals helps
Evidence
- Laying groundwork for an ILOS program that includes medically tailored meals
Pilot Program Reporting
- Preparing data for internal and external stakeholders including state Medicaid directors and state departments of health
Pilot Program Development
- Identifying targeted members
- Developing protocols
- Measuring outcomes
ILOS Program Definition
- Eligible populations
- Credentialing
- Billing requirements
Resources for you
Considering ILOS for your plan but need support?
The Mom’s Meals team can help. Contact John Phillips, vice president, business development at john.phillips@momsmeals.com or 888-343-8020.
Updated white paper offers ways to break down barriers to innovation

Innovating to Overcome Food Insecurity shows how states are taking new approaches to achieve better outcomes. Discover how programs can accommodate current day challenges — yet innovate — when addressing community-based hunger with:
- Government and state challenges and opportunities
- Case studies of state-level success
- 5 questions to answer to get successfully started
.jpg)

